Contents
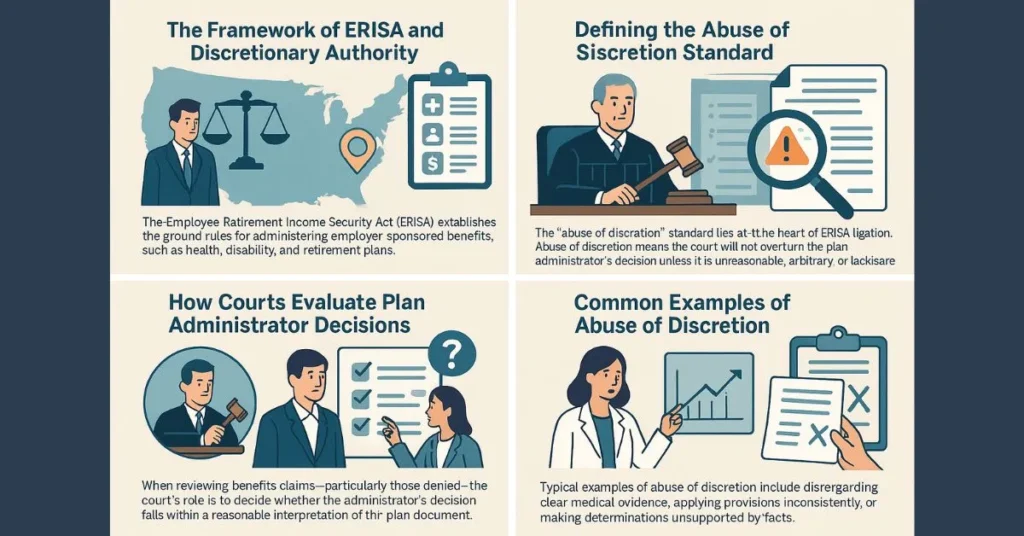
- The Framework of ERISA and Discretionary Authority
- Defining the Abuse of Discretion Standard
- How Courts Evaluate Plan Administrator Decisions
- Common Examples of Abuse of Discretion
- The Role of Documentation and Process
- Recent Legal Developments
- Best Practices for Participants and Administrators
- Trends Impacting the Abuse of Discretion Standard
The Framework of ERISA and Discretionary Authority
The Employee Retirement Income Security Act (ERISA) establishes the ground rules for administering employer-sponsored benefits, such as health, disability, and retirement plans. ERISA is designed to protect plan participants by setting minimum standards for plan management. A defining feature of many ERISA-governed plans is the discretion plan administrators have in interpreting plan terms and making benefits decisions. This discretion often becomes central when participants challenge denials or interpretations. To navigate the legal landscape and understand plan rights, resources like https://www.benefitslaw.com/ offer helpful guidance on key ERISA principles and emerging issues.
Employers and insurance carriers acting as plan administrators commonly reserve the authority to interpret the plan and determine eligibility for benefits. This reservation of authority influences how courts assess disputed claims. Understanding the division between administrative discretion and statutory duty is essential for anyone involved with an ERISA plan, as courts use these boundaries to determine whether plan decisions should stand or be overturned.
Defining the Abuse of Discretion Standard
The “abuse of discretion” standard lies at the heart of ERISA litigation. When a plan document specifically grants the administrator discretionary authority, courts typically review a challenged decision under this deferential standard. Abuse of discretion means the reviewing court will not overturn the plan administrator’s decision unless it is unreasonable, arbitrary, or lacks substantial evidence. This protective approach is quite distinct from de novo review, where the court takes a fresh look without deferring to the administrator’s judgment. Under abuse of discretion, the administrator’s interpretation is upheld as long as it’s rational and follows the plan’s terms.
Courts consider the administrator’s expertise, the complexity of the plan language, and the consistency of decisions over time. The idea is to respect the intent of the plan drafters while safeguarding participants from unfair or capricious decisions. As such, the standard aims to balance judicial oversight with the practical need for plan sponsors to have flexibility in managing benefits.
How Courts Evaluate Plan Administrator Decisions
When reviewing benefits claims—particularly those denied—the court’s role is to decide whether the administrator’s decision falls within a reasonable interpretation of the plan document. Courts evaluate whether the decision was supported by substantial evidence and whether the process was fair. They do not substitute their judgment but assess whether the administrator considered all the relevant information.
Important factors in the review include the clarity of the plan’s terms, whether procedures were followed, and whether the claim evaluation was consistent with prior similar cases. Courts also weigh any potential conflict of interest, such as when an insurer decides and pays claims. The presence of a conflict does not automatically result in a ruling against the administrator, but may tilt the analysis if evidence of bias appears.
Common Examples of Abuse of Discretion
Not every denial or disputed interpretation amounts to abuse of discretion. Typical examples include disregarding clear medical evidence, applying provisions inconsistently, or making determinations unsupported by facts. Suppose a plan administrator ignores a treating physician’s opinion in favor of a less credible report or fails to clearly explain a denial in an adverse benefit determination. In that case, courts may find abuse of discretion.
Other mistakes leading courts to intervene include using outdated plan documents, not following claims procedures, or failing to communicate clearly to the participant. Documented inconsistencies in similar cases or repeated errors across claims may signal abuse of discretion and invite closer judicial scrutiny.
The Role of Documentation and Process
Detailed, timely documentation is critical in defending plan decisions. Administrators should record all considered evidence, reasons for the decision, and communications with the participant. Strong documentation demonstrates that the plan acted within its discretion, adhering to the plan terms and federal regulations.
Process matters as much as substance. Following established claims procedures, clearly communicating adverse decisions, and respecting appeals timelines are necessary. Courts consider whether participants were given a full and fair process as ERISA requires when evaluating claims of abuse of discretion. Adherence to best practices can help reduce litigation risk for plan sponsors.
Recent Legal Developments
Court interpretations of the abuse of discretion standard evolve with new rulings and regulatory developments. High-profile cases continue to refine the boundaries and expectations placed on administrators, including the duty to review all claim materials and explain denials in detail. Developments highlighted in recent HR news reflect broader trends toward requiring greater transparency and fairness in plan administration.
In response, many courts demand a deeper explanation from plan administrators when denying benefits. Recent Department of Labor efforts have also reinforced the need for written guidelines and claims handling training, especially regarding disability decisions. This evolving landscape means administrators and participants must stay informed on case law and agency updates to protect their interests.
Best Practices for Participants and Administrators
For plan participants, understanding your rights, reviewing all plan materials, and requesting written decisions are essential first steps if benefits are denied. Detailed records and timely appeals improve the chances of a favorable outcome should litigation arise. Participants should also utilize available resources and support networks to ensure every claim receives appropriate consideration.
Administrators can reduce challenges and litigation by providing clear, consistent explanations for decisions, proactively documenting each step and training staff on ERISA compliance. Incorporating guidance from trusted sources, such as reliable HR resources, can also improve plan operations and transparency. Open communication and diligent adherence to the process foster trust and minimize misunderstandings.
Trends Impacting the Abuse of Discretion Standard
Several ongoing trends will likely impact the abuse of discretion standard for years. With a greater focus on employee well-being, courts and regulators are emphasizing transparent, participant-friendly procedures. Legislative changes and new Department of Labor regulations continue to raise expectations for plan fairness and thoroughness in claim reviews.
Advances in digital recordkeeping and claims processing can help administrators meet higher accountability standards. However, as technology evolves, so does the scope of what’s possible and required in plan administration. Both plan sponsors and beneficiaries benefit from staying updated on these trends to ensure protection and fair treatment under ERISA.