In the dynamic complex environment of healthcare, especially during interaction between healthcare providers and patients, it is crucial to use language that is comprehensible and unambiguous.
Practitioners can best uphold a high level of communication and support a holistic approach to patient care through the use of SOAP notes. With this knowledge of what a SOAP note is, guidelines on how to use a SOAP note can thus improve the delivery of care and hence the patient outcomes.
Contents
What is a SOAP Note?
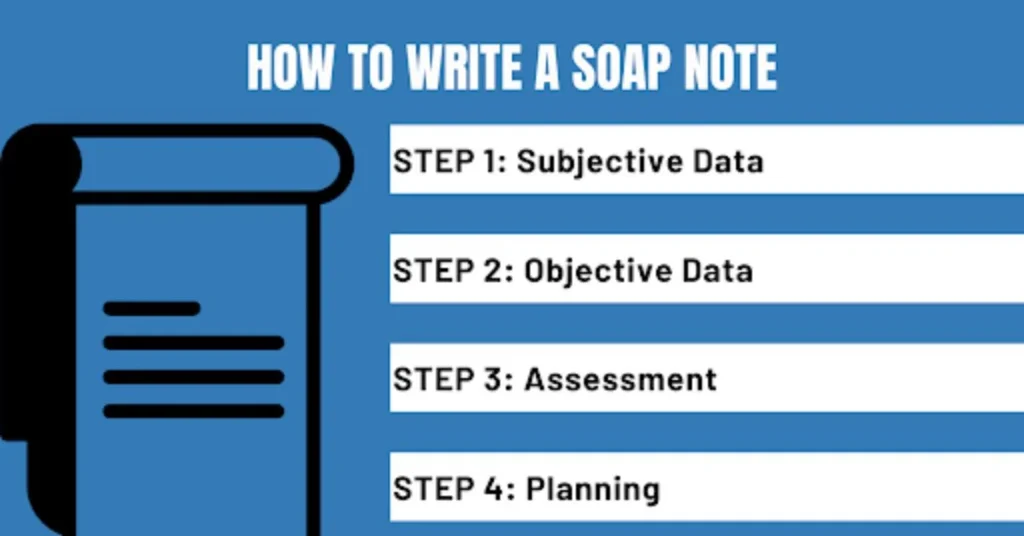
SOAP note on the other hand is a documentation format of the patient where information is presented in a prescribed format. SOAP is an acronym that carries the following meaning; S for subjective, O for objective, A for assessment, and P for plan.
SOAP notes were designed to prevent loss of patient information during treatment and enable all staff involved in patient care to take notes simultaneously in an organized and understandable manner. Each letter in SOAP serves a specific purpose, aiming to provide a comprehensive understanding of the patient and the care provided.
The SOAP Note Format
The SOAP note format is designed to streamline the documentation process and ensure that all critical aspects of a patient’s care are recorded. Here’s a breakdown of the sections:
- Subjective (S): This section includes the patient’s reported symptoms, feelings, and concerns. Capturing the patient’s perspective is essential as it provides context for the objective findings.
- Objective (O): Here, healthcare providers document measurable and observable data such as vital signs, physical examination findings, and results from diagnostic tests. This section focuses on factual information.
- Assessment (A): This part of the note involves the healthcare provider’s clinical judgment and diagnosis based on the subjective and objective information. It’s a synthesis of the data collected.
- Plan (P): The plan section of the SOAP note outlines the proposed treatment and follow-up actions. This may include medications, therapies, further testing, and patient education.
The Importance of SOAP Notes in Care Coordination
Enhancing Communication in Care
Interprofessional collaboration relies on the ability of clinicians to communicate effectively when managing patients who are receiving care from numerous healthcare workers. SOAP notes lead to structured documentation, enhancing efficiency by ensuring that every provider has equally detailed information.
This minimizes the chances of passing incorrect information and ensures that each team member understands every aspect of the patient’s status and the next course of action.
Providing Continuity of Care
Continuity of care is crucial for effective patient management. SOAP notes allow a proper patient map and an equitable record of the patient’s interactions, treatments, and progress.
New providers can easily assess the patient’s history, diagnosis, and overall assessment upon joining the care team. Patient needs vary, emphasizing the importance of addressing them appropriately to ensure competent care.
Facilitating Evidence-Based Practice
SOAP notes enable a practitioner to use EBP since details on any objective data and or clinical assessments are captured.
This is useful for the providers as they can see the impact of treatments administered to the learning disabled and make further amendments based on the documented notes. It makes it possible to base patient management on scientific evidence and professional judgment at all phases of their treatment.
How to Write SOAP Notes Effectively
Subjective Section
When documenting SOAP notes, begin with the subjective assessment section. Take writing from the patient of the patient’s complaints, symptoms, and then what concerns the patient has.
Use probing responses that will give detailed answers to the questions posed. For instance, “Tell me more about the pain you’re feeling?” Or, “What has your state of health been since your previous visit? The subjective section lays the groundwork for the objective findings.
Objective Section
When writing in the objective section one should measure and record Data that is quantifiable and observable. This includes data on the patient’s general health status reflected in vital signs, findings from physical examinations, and data from diagnostic procedures. Avoid using general and vague terms, especially when referring to key results.
Assessment Section
This section consists of an assessment that entails clinical decision-making. Here, tailor the numerical data together with clinical impressions or feelings to make a diagnosis or clinical impression. Be concise but comprehensive.
Plan Section
The evaluation, also known as the PLAN section of the SOAP note, captures the next steps regarding the patient’s care. These are treatments, medicines, other examinations, and checkups that one has to undergo after the disease is detected.
Benefits of the SOAP Charting Method
Improved Documentation
The SOAP charting method enhances documentation and organizes comprehensive records. SOAP notes divide the work into specific segments, simplifying the process of finding and interpreting information. This thought process is expected to enhance the uniformity of patient record-keeping and management.
Legal and Ethical Compliance
This is vital as it helps with legal and ethical concerns in the documentation process of events, patient records, and other paperwork.
Employee notes contain all the records, including the SOAP note, and effectively summarize the patient’s case and caregiving interactions as needed in court cases. They also facilitate documentation of care in a manner that adheres to professionalism and applicable legislation.
Enhanced Training and Education
Healthcare students and trainees must learn how to write SOAP notes correctly. Using the SOAP note format enables healthcare workers to be systematic and develop critical thinking skills in patient care. It also prepares them for clinical practice scenarios, where documentation is paramount.
Interdisciplinary Collaboration
SOAP notes are valuable for patient care teams because they provide a standardized and efficient method of documentation across various health disciplines.
SOAP notes can be adopted by all caregivers in the healthcare field like doctors, nurses, physical therapists, and the like to attain a rapid exchange of information. The two approaches are synergistic and remain critical for total patient care.
Conclusion
SOAP notes are undeniably essential in acute care settings today, as they enhance care coordination, communication, and continuity of care.
By learning about the SOAP note and its application, how to write proper SOAP notes, and incorporating the SOAP note structure, healthcare practitioners can improve the quality of diagnostics and treatment, benefiting the patients.
From a legal and ethical perspective, the SOAP charting method is invaluable. It provides a significant boost to staff training and interdisciplinary teamwork, facilitating the development of professional documentation knowledge and practice for healthcare workers.
Despite the ever-growing development and advancement in nursing care models, the use of SOAP remains a vital tool for patient analysis and management in healthcare institutions.
FAQs
- What are some tips for writing effective SOAP notes?
Tips for writing effective SOAP notes include being concise and precise, using specific and quantifiable terms in the objective section, synthesizing information clearly in the assessment, and outlining detailed and actionable steps in the plan section.
- Can SOAP notes be used in all healthcare settings?
Yes, SOAP notes can be used in a wide range of healthcare settings, including hospitals, clinics, private practices, and more. Their standardized format makes them adaptable to various healthcare environments and specialties.
- Are there any common mistakes to avoid when writing SOAP notes?
Common mistakes to avoid when writing SOAP notes include being too vague or verbose, failing to update the notes regularly, omitting critical information, and not following the structured format.